Posterior Cruciate Ligament Injury (PCL)
The posterior cruciate ligament (PCL) is the strongest ligament in the knee, crucial for stabilising the joint by preventing the tibia from moving backward relative to the femur. An injury to this ligament can range from a minor stretch to a complete tear, often resulting from trauma or excessive force applied to the knee.
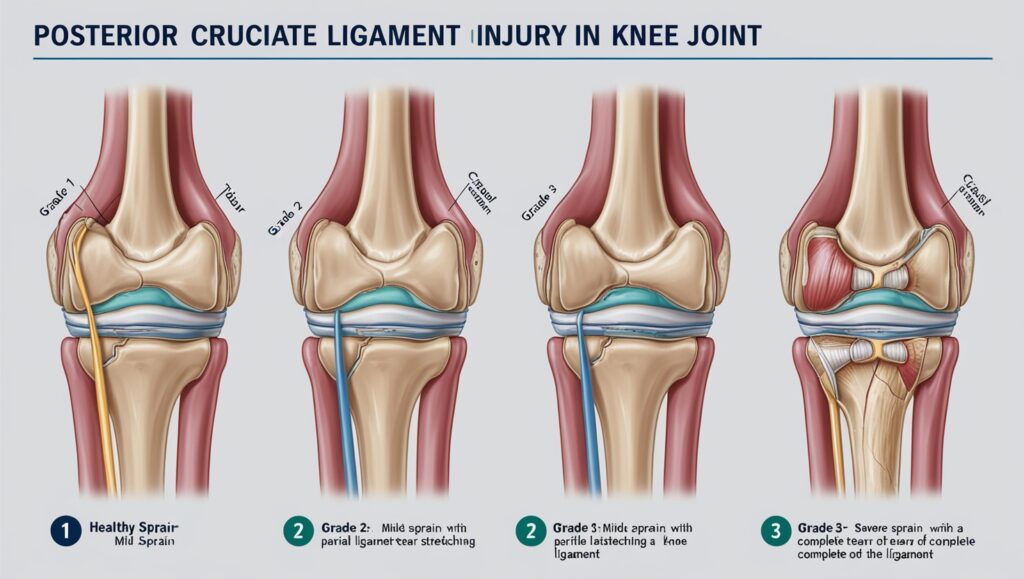
Grade Classification
- Grade I PCL Sprain: This is a mild sprain characterised by a small partial tear of the ligament. Typically, there is minimal pain and no significant instability in the knee. Tibial translation (backward movement of the tibia relative to the femur) is 1-5 mm.
- Grade II PCL Sprain: This grade indicates a moderate sprain, where more than 50% of the ligament is usually torn. The knee may feel loose but is not necessarily unstable. Tibial translation ranges from 6-10 mm, indicating a significant injury that may require close monitoring.
- Grade III PCL Tear: This indicates a complete tear of the PCL, where the ligament is no longer functional. It often occurs in conjunction with injuries to other ligaments in the knee, such as the lateral collateral ligament (LCL). Tibial translation is greater than 10 mm and patients experience significant instability in the knee, making it difficult to perform activities such as climbing stairs or pivoting.
Causes:
PCL injuries typically arise from:
- Direct Trauma: A common cause includes a bent knee striking a dashboard during a car accident.
- Sports Injuries: Falling on a bent knee or twisting injuries during sports can also lead to damage.
- Hyperextension: Landing awkwardly after jumping may cause hyperextension of the knee, resulting in PCL injury.
Symptoms
Individuals with a PCL injury may experience:
- Pain and swelling that develops quickly after the injury.
- Stiffness in the knee, leading to difficulties in walking.
- A sensation of instability, as if the knee might “give out.”
Diagnosis and Management
Diagnosis often involves a complete physical examination, which includes specific tests such as the posterior drawer test. Imaging tests, such as MRI, may be performed to assess the extent of the injury. Management strategies include:
- Initial Care: Immediate first aid using the RICE method (Rest, Ice, Compression, Elevation) is essential.
- Immobilisation: A brace may be used to stabilise the knee and prevent further injury.
- Physical Therapy: Rehabilitation focuses on restoring strength and mobility through targeted exercises.
Treatment Options
Treatment varies based on injury severity:
- Non-Surgical Treatment: Isolated grade I or II injuries often heal well without surgery. Patients typically engage in physical therapy and may return to sports within weeks.
- Surgical Treatment: For severe injuries or combined ligament tears, surgical reconstruction of the PCL may be necessary. This procedure usually involves using grafts from other tissues.
Medication
Pain relief and inflammation reduction can be managed with over-the-counter medications such as NSAIDs (e.g., ibuprofen). Doctor’s prescription medications may be necessary for pain management.
Precautions
To prevent future injuries:
- Engage in proper warm-up and stretching before physical activities.
- Strengthening exercises for leg muscles, particularly the quadriceps and hamstrings, can enhance knee stability.
- Avoid high-risk sports or activities if previously injured.
How Does a Posterior Cruciate Ligament Injury Affect My Body?
PCL injuries can significantly impact mobility and stability. Patients may experience persistent pain and instability in the knee joint, which can affect daily activities and athletic performance. If left untreated or poorly managed, altered biomechanics can lead to the development of chronic knee problems, including arthritis and increased stress on other knee structures.
In summary, understanding PCL injuries is important for effective prevention and management. Early diagnosis and appropriate treatment can lead to favorable outcomes and a return to normal activity.
Consequences of Chronic PCL Injuries
- Increased Tibial Translation: Chronic PCL injuries can result in increased back-and-forth sliding of the tibia relative to the femur, leading to instability in the knee joint.
- Meniscal Tears: There is a heightened risk of medial (inner) meniscal tears due to the altered mechanics of the knee caused by PCL deficiency.
- Arthritis Development:
- Medial Knee Arthritis: Studies indicate that around 80% of patients may develop arthritis in the medial compartment of the knee within five years following a PCL tear.
- Patellar Arthritis: Similarly, about 50% of individuals may experience arthritis behind the patella (kneecap) within the same timeframe.
- Pain and Functional Limitations: Patients with chronic PCL injuries often report pain localised at the medial aspect of the knee, particularly due to associated meniscal tears and arthritis. This pain can be exacerbated during activities such as descending stairs or slopes, and during turning or pivoting movements.
- Instability and Functional Impairment: Individuals may experience significant knee instability, which can lead to difficulties in performing everyday activities, especially those involving sudden movements or changes in direction.
Long-term Prognosis
The long-term prognosis for individuals with chronic PCL injuries is particularly related to joint health. Cartilage degeneration is more likely, with a 75% chance of developing a tear in the medial femoral condyle and a 50% chance of developing a tear behind the patella within five years of injury. Overall, chronic PCL injuries can significantly impact quality of life and level of physical activity, making early diagnosis and appropriate management crucial to minimise these consequences.