You need to know about ADHA (Attention deficit hyperactivity disorder) ?
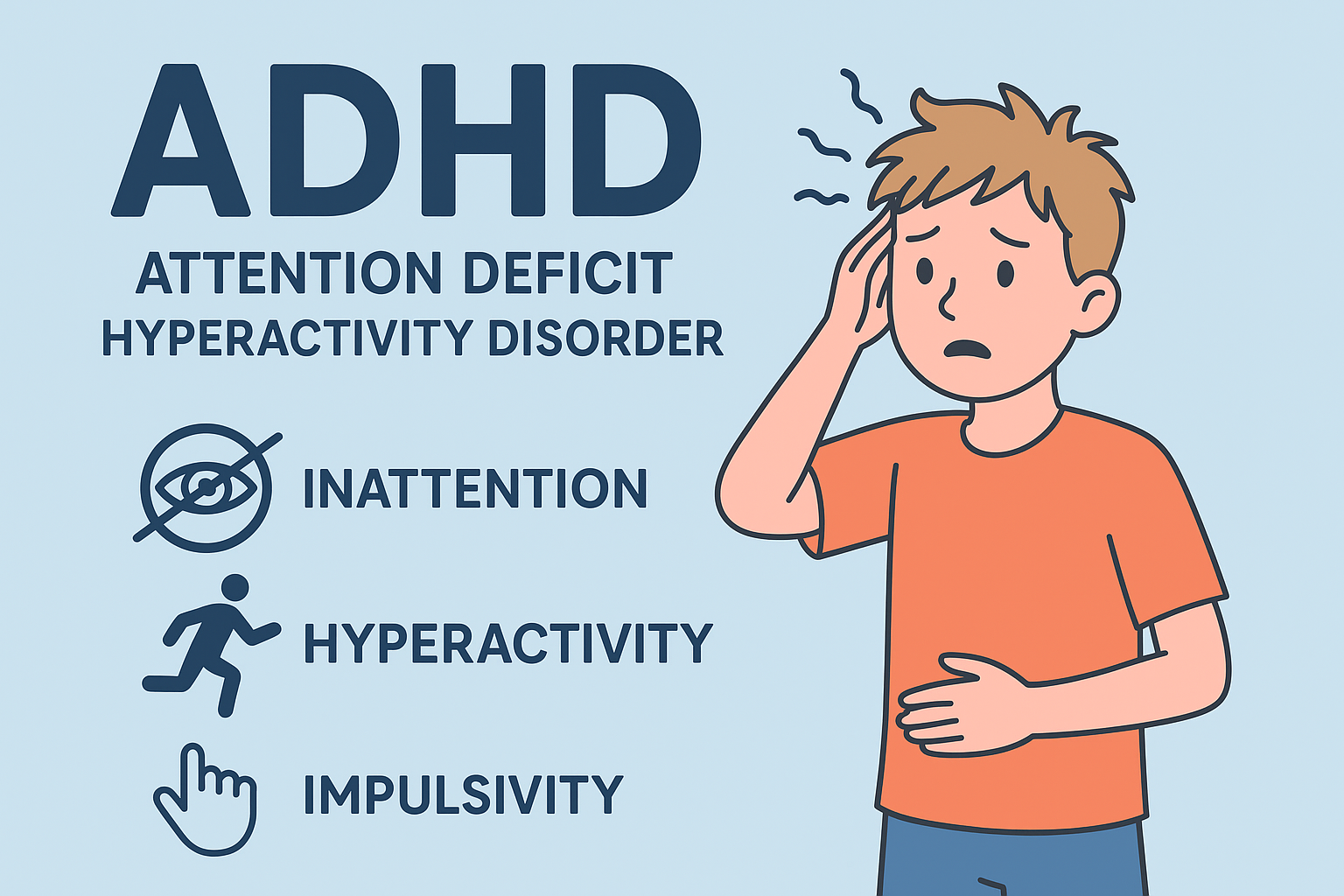
ADHA (Attention Deficit Hyperactivity Disorder) . ADHD is a neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, and impulsivity. It can affect various aspects of life, including academic performance, work, and relationships.
- Inattention: This includes difficulty sustaining attention, frequent careless mistakes, difficulty organizing tasks, and being easily distracted.
- Hyperactivity: Symptoms include excessive fidgeting, difficulty remaining seated, and a tendency to talk excessively.
- Impulsivity: This involves making hasty decisions without considering the consequences, interrupting others, and having trouble waiting for one’s turn.
ADHA (Attention Deficit Hyperactivity Disorder) is commonly diagnosed in childhood, but its symptoms can continue into adolescence and adulthood. Treatment often involves a combination of behavioral therapies, medication, and lifestyle adjustments to help manage symptoms and improve functioning.
Types of ADHA
- Predominantly Inattentive Presentation:
- Symptoms: Difficulty sustaining attention, following through on tasks, organizing activities, and avoiding distractions.
- Characteristics: Individuals might seem daydreamy, forgetful, or disorganized, but may not show significant hyperactive or impulsive behaviors.
- Predominantly Hyperactive-Impulsive Presentation:
- Symptoms: Excessive fidgeting, restlessness, difficulty remaining seated, excessive talking, and acting without considering consequences.
- Characteristics: Individuals may struggle with waiting their turn, interrupt others, or have difficulty engaging in activities quietly.
- Combined Presentation:
- Symptoms: A mix of both inattentive and hyperactive-impulsive symptoms.
- Characteristics: Individuals exhibit significant symptoms from both categories, leading to a combination of issues with focus, organization, impulsivity, and excessive activity.
Symptoms of ADHA (Attention Deficit Hyperactivity Disorder)
ADHD symptoms fall into two main categories: inattention and hyperactivity-impulsivity. These symptoms can vary in severity and may present differently in adults compared to children.
1. Inattention
- Difficulty sustaining attention: Trouble focusing on tasks or activities for extended periods.
- Careless mistakes: Frequent errors in schoolwork, work, or other activities due to a lack of attention to detail.
- Difficulty organizing tasks: Struggles with managing time, keeping track of tasks, and maintaining order.
- Avoiding tasks requiring sustained mental effort: Procrastination or avoidance of tasks that require prolonged concentration.
- Easily distracted: Frequent interruptions by external stimuli or unrelated thoughts.
- Forgetfulness: Frequently forgetting daily activities, appointments, or obligations.
2. Hyperactivity-Impulsivity
- Fidgeting or tapping: Restlessness, such as tapping hands or feet or shifting in one’s seat.
- Difficulty remaining seated: Getting up from one’s seat in situations where remaining seated is expected.
- Running or climbing in inappropriate situations: Engaging in excessive physical activity or movement when it’s not suitable.
- Inability to play or engage in activities quietly: Trouble playing or engaging in activities quietly or calmly.
- Excessive talking: Talking more than what is typical or expected in various situations.
- Interrupting or intruding: Interrupting others, finishing their sentences, or speaking out of turn.
- Difficulty waiting for one’s turn: Impatience and difficulty waiting for one’s turn in various situations.
What Causes of ADHA (Attention Deficit Hyperactivity Disorder)
1. Genetic Factors
- Hereditary: ADHD tends to run in families, suggesting a genetic component. Studies show that if a parent has ADHD, their child is at a higher risk of having it too.
2. Brain Structure and Function
- Neurodevelopmental Differences: Brain imaging studies have found differences in the structure and function of the brains of individuals with ADHD. These differences are often seen in areas responsible for attention, impulse control, and executive function.
- Neurotransmitter Imbalances: There is evidence suggesting that imbalances in neurotransmitters, such as dopamine and norepinephrine, may play a role in ADHD.
3. Prenatal and Early Life Factors
- Exposure to Toxins: Prenatal exposure to tobacco smoke, alcohol, and certain drugs has been linked to an increased risk of developing ADHD.
- Premature Birth or Low Birth Weight: Babies born prematurely or with a low birth weight may be at higher risk.
- Maternal Stress: High levels of stress or complications during pregnancy can contribute to the development of ADHD.
4. Environmental Factors
- Lead Exposure: Exposure to lead, particularly during early childhood, has been associated with an increased risk of ADHD.
- Family Environment: While family dynamics and parenting styles can influence behavior, they are not considered direct causes of ADHD. However, they can impact the severity and management of symptoms.
5. Other Factors
- Diet and Nutrition: Some studies suggest that certain dietary factors or deficiencies might exacerbate symptoms, though they are not considered primary causes of ADHD.
- Sleep Problems: Sleep disturbances can mimic or exacerbate ADHD symptoms, but they are not typically seen as a cause.
Diagnosis of ADHA (Attention Deficit Hyperactivity Disorder)
- Clinical Evaluation
- Medical History: Includes a thorough review of the individual’s health history and family background.
- Symptom Assessment: Detailed examination of symptoms according to the DSM-5 criteria, including the type, duration, and severity of symptoms.
- Diagnostic Criteria (DSM-5)
- Inattention: Symptoms such as difficulty sustaining attention, frequent careless mistakes, and organizational problems.
- Hyperactivity-Impulsivity: Symptoms such as excessive fidgeting, restlessness, and difficulty waiting one’s turn.
- Age of Onset: Symptoms must be evident before age 12.
- Duration and Impact: Symptoms must persist for at least six months and cause significant impairment in social, academic, or occupational functioning.
- Additional Assessments
- Behavioral Checklists: Use of standardized tools like the Conners’ Rating Scales or Vanderbilt Assessment Scales.
- Input from Multiple Sources: Collecting reports from parents, teachers, and other caregivers.
- Rule Out Other Conditions
- Differential Diagnosis: Exclude other conditions with similar symptoms, such as anxiety disorders, depression, or learning disabilities.
Treatment of ADHA (Attention Deficit Hyperactivity Disorder)
Treatment typically involves a combination of approaches tailored to the individual’s needs:
- Medication
- Stimulants: The most commonly prescribed medications, including methylphenidate (e.g., Ritalin) and amphetamines (e.g., Adderall). They help increase attention and decrease hyperactivity and impulsivity.
- Non-Stimulants: Options like atomoxetine (Strattera) and guanfacine (Intune) are used when stimulants are ineffective or cause undesirable side effects.
- Behavioral Therapy
- Cognitive Behavioral Therapy (CBT): Helps individuals develop coping strategies, improve organization, and manage emotions.
- Behavioral Interventions: Focus on modifying specific behaviors, using rewards and consequences to reinforce positive behaviors.
- Educational Interventions
- Special Education Services: Tailored support in the classroom, including accommodations like extended time for tests and a structured learning environment.
- Organizational Strategies: Teaching time management skills and organizational techniques.
- Parent Training and Family Therapy
- Parent Training: Educates parents on effective behavior management strategies and how to support their child’s needs.
- Family Therapy: Addresses family dynamics and helps improve communication and support within the family.
- Lifestyle Adjustments
- Routine and Structure: Implementing consistent routines and structured environments to help manage symptoms.
- Healthy Habits: Encouraging regular physical activity, a balanced diet, and adequate sleep.
- Psychoeducation
- Understanding ADHD: Educating the individual and their family about ADHD to improve understanding and support.